Traumatic Brain Injury: What Happens Next?
More efficient classification and predictive models could lead to better treatment for traumatic brain injuries.

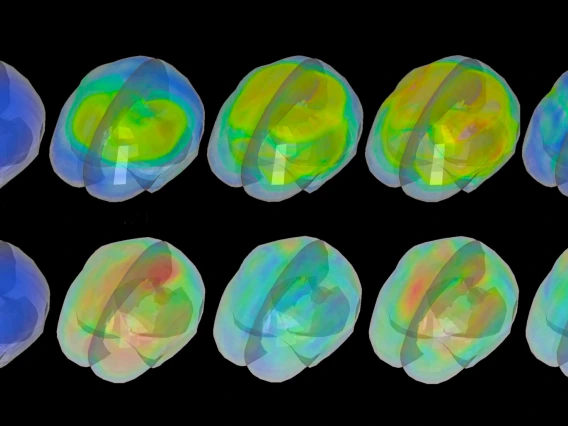
No description provided
When a patient sustains a traumatic brain injury, or TBI, and is admitted to a trauma center, clinicians classify the severity of the injury as either mild, moderate or severe -- the same way they assess the consciousness level of anyone who walks into the emergency room.
But the differences between TBIs, from when they first happen to the days following the primary injury to their outcomes years later, are hugely variable. One side effect of using such broad classifications for these injuries is that clinicians are unable to reliably predict both short-term and long-term outcomes for patients.
“Every traumatic brain injury is unique,” said Vignesh Subbian, an assistant professor in the Department of Biomedical Engineering, or BME, and the Department of Systems and Industrial Engineering, or SIE, and a member of the BIO5 Institute at the University of Arizona. “Let’s say two people fall down the stairs the same way and get hit in the exact same place. They’re still going to have different traumatic brain injuries. We can’t change what happened -- the primary injury -- but there is room to prevent further damage to the brain.”
Subbian is principal investigator on a new grant of just over $500,000 from the National Science Foundation, or NSF, to help better characterize TBIs and predict their outcomes -- and therefore, more effectively treat them. This grant brings together key researchers and clinicians from other institutions, including Emory University, the University of Cincinnati and Virginia Tech, with nearly $1.2 million in support from NSF overall.
“This NSF award exemplifies a successful collaboration among systems and industrial engineering, biomedical engineering, computer science and health sciences to work on a complex, interdisciplinary problem that has a high impact on our society,” said Young-Jun Son, department head of SIE. “I am very proud of Dr. Subbian for leading this exciting project.”
With traumatic brain injury as the leading cause of death and disability for individuals under age 44, and an estimated 1.7 million cases occurring in the United States every year, it’s an area in dire need of better predictive tools and further research.
“TBIs pose a significant public health burden, often resulting in long-term disability and poor quality of life,” said Subbian, who has been working in TBI research for nearly eight years.
Delving Into Large Clinical Datasets
Using analytical techniques and data gathered from advanced monitoring of brain injury patients, researchers will develop methods to better classify TBI patients and predict what might happen next.
“This will allow clinicians to provide the right care to the right TBI patient at the right time,” Subbian said.
Currently, if patients survive their time in the intensive care unit, the extent of their recovery is uncertain. The tools developed through this research would allow for targeted allocation of resources and help set expectations for family members and other caregivers. It could also inform clinical researchers on how to select patients for traumatic brain injury clinical trials, 100 percent of which have failed over the past 30 years.
“In the future, we might be able to identify patients best suited for specific TBI clinical trials,” Subbian said. “Not accounting for the wide variation in TBI cases is one of the reasons all clinical trials failed in the past.”
A Stepping Stone to Wider Applications
Although this work will initially be focused on TBIs, the methods researchers develop will be applicable to other critically ill patients, such as those with cardiovascular disorders.
“This project is a stepping stone,” Subbian said. “We’re going to use this project to generate a wide range of prototypical tools, and then we’re really going to push for generalizability.”
This research is funded by the Smart and Connected Health Program, a partnership between multiple federal agencies, including NSF and the National Institutes of Health, or NIH, that aims to transform health and medicine by integrating methods from different disciplines, including computing and information sciences and engineering. Subbian, who is the university’s first and only joint appointee between the BME and SIE departments, serves as a bridge between computational and systems engineering methods and biomedical problems.
“NSF and NIH developed this program to catalyze multidisciplinary collaborations and facilitate fundamental, integrative research that will address large, grand-challenge problems in medicine and healthcare,’” Subbian said. “Our project is an example of one of the cross-cutting areas I was recruited to lead.”
BME department head Art Gmitro said Subbian has been a fantastic addition to the department’s faculty, and that he couldn’t agree more.
“Not only has he developed an active research program in the area of medical informatics and health care systems engineering, as evidenced by this grant, but he has also proven to be an outstanding teacher and mentor for our students,” he said. “Both the Department of Biomedical Engineering and the Department of Systems and Industrial Engineering are proud to have him as a member of our faculty.”